
(Aidan took the course Health Interprofessional 408: Cultural Safety and Health: Indigenous Perspectives, prior to starting his SSRP. The course focused on colonialism, reconciliation, cultural safety, and a community visit to the Okanagan Indian Band. The Pit House above is a place of ceremony, celebration, gatherings, and sharing of knowledge. It was hand-made by Elder Eric Mitchell, one of the course Knowledge Keepers.)
Aidan O’Callahan, an Honours Cognitive Psychology and Indigenous Studies student from the University of British Columbia Okanagan, worked on a FoM SSRP research project in the summer of 2019.
Could you please briefly describe the project you were involved with?
AO: For sure! Over the summer, I worked under Dr. Charlotte Jones (clinical associate professor of endocrinology and Director of Student Research at the Southern Medical Program) and Dr. Donna Kurtz (associate professor of nursing, cultural safety expert and Indigenous scholar), who have been leading a groundbreaking project aimed at providing culturally safe and effective diabetes and obesity interventions for Urban or “off-reserve” Indigenous Peoples through telehealth.
Urban Indigenous Peoples account for roughly 60% of Indigenous Peoples in B.C. (Census 2016) and face unique barriers in accessing health and wellness resources, given disparities between on-reserve and off-reserve public health capacity.
As outlined by the Canadian Institutes of Health Research (CIHR) and the Public Health Agency of Canada (PHAC), the combination of higher rates of diabetes, obesity and related complications is one of the four urgent Indigenous health challenges (Indigenous Pathways for Diabetes and Obesity, 2018). Therefore, the goal of our project was to bring together Traditional Indigenous and Western knowledge to improve diabetes and obesity wellness within off-reserve Indigenous communities.
What is “telehealth”?
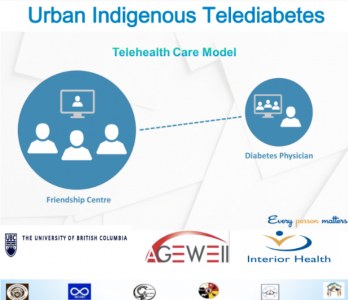
(Adapted from Susi Wilkinson)
AO: Telehealth can be thought of as a way of connecting diabetes/obesity specialists with patients in a different location via videoconferencing software. Within our project, the communities as well as our research team envisioned patients at a local Friendship Centre having a nurse by their side to perform evaluations, treatments and health education while simultaneously consulting with health practitioners specializing in obesity/diabetes. Utilizing the Friendship Centres allows patients to access their telediabetes/obesity needs in a culturally safe environment while providing opportunities for Traditional healing and community engagement.
Why were you interested in pursuing this project?
AO: Some of my very first memories come from the Puyallup Tribe in Washington State, and I am privileged to currently live and study on the unceded and ancestral territory of the Syilx People. I’m committed to a lifelong journey of learning and practicing cultural safety and allyship, and I am honored to work with Indigenous and non-Indigenous healthcare professionals to bridge the healthcare disparities that Indigenous Peoples face on a daily basis. I’m passionate about the need for reconciliation, especially in our current healthcare system, and telehealth is one of the avenues that is being pursued to bridge the healthcare gap for Indigenous Peoples and communities.

(The research team for Indigenous methodologies: Building capacity for obesity/diabetes TeleHealth care in Urban (and rural) Indigenous communities (I’M T’CARE). In the front from left to right is Dr. Donna Kurtz; Elder Jessie Nyberg; Dr. Charlotte Jones. In the back from left to right is Karim Davarani; Aidan O’Callahan; Dr. Julianne Barry; Chella Percy.)
What are some things you learned along the way?
AO: From a surface level, I learned a lot about telehealth implementation and delivery, but the most important learning moments I had during this project were really with Elders, Indigenous physicians, community members and my two supervisors. In Prince George, I had the opportunity to experience first-hand how Carrier Sekani Family Services were able to transform the dynamic of health care for the Indigenous communities they work with through telehealth. During our visit, we were all humbled to meet and collaborate with Dr. Clayton Reynolds and Dr. Terri Aldred, who were able to share their extensive knowledge and experiences in rural medicine, telehealth and serving Indigenous communities.
In Kamloops, I had the opportunity to meet with leaders and practitioners within the six Urban Indigenous communities we were working with. The spirited dialogue and collaboration reinforced to me how we were all united in working towards improving healthcare outcomes for patients with obesity and/or diabetes right now and for our future generations. I’m inspired by the hard work that has already gone into this unique project, in bringing together diverse groups and perspectives to collaborate on creating meaningful advancements in healthcare.
The most insightful part of this project was watching Dr. Jones and Dr. Kurtz come together to brainstorm and integrate their unique talents to embark on ambitious multidisciplinary research. The amazing collaborative spirit in bringing people together inspired me to pursue a career in medicine, where I feel I can use my skills and experiences to create the biggest impact towards improving Indigenous and non-Indigenous healthcare outcomes. Dr. Donna Kurtz was my other mentor during the summer, and I was fortunate enough to take her course on Indigenous cultural safety in health before the start of this project (UBC-O HINT 408). Dr. Kurtz is a brilliant Métis nurse educator and expert on cultural safety and her course provided me with an opportunity to expand my knowledge and awareness before embarking on my FoM SSRP project.
Dr. Charlotte Jones is a clinical associate professor at the University of British Columbia’s Southern Medical Program and a practicing endocrinologist. She supervised the project Aidan participated in along with her co-Principal Investigator Dr. Donna Kurtz.
How was Aidan able to help as part of the research team?
CJ: Aidan has been a wonderful addition to our project. Aidan helped to co-design and obtain Accreditation for a diabetes/obesity specialized training course for general practitioners (GPs) as a facet of the three year grant: Indigenous Methodologies: Building Capacity for Telediabetes Care in Urban Indigenous Communities. I, along with another endocrinologist and an Indigenous family doctor, developed the core curriculum competencies while Aidan helped with the structure of the course and also constructed our application to get it approved by the Royal College of Physicians and Surgeons. This was a very intensive process and Aidan had to work hard to meet the high standards necessary for approval. He is also in the process of finishing a manuscript on our project’s unique methodologies and telehealth approach.
How do you think this opportunity has impacted Aidan?
CJ: This opportunity has certainly allowed Aidan to further explore his passion for healthcare, telehealth research, and Indigenous methodologies. He met with many Indigenous and non-Indigenous physicians, nurses, and academics over the summer months and now has extensive exposure to this important, emerging area within healthcare. He is also working towards becoming a Highly Qualified Professional (HQP) with our federally-funded Networks of Centres of Excellence (NCE) organization, AGE-WELL. In doing so, he has participated in webinars about inclusion in science and healthcare, taken online modules on a variety of topics, and has completed multiple certifications on cultural safety and ethical practices in science. He has been awarded funding through UBC-O’s Multidisciplinary Research Projects in Health (MURPH) program for 2019/2020 and will continue to work on our project. He will be presenting this work at three different conferences this year, including both oral and poster presentations. We’re all very excited for his future accomplishments.
How was it working with Aidan and supporting his SSRP?
CJ: Working with Aidan has been a great pleasure. He’s consistently enthusiastic, hardworking and a great communicator. It has been wonderful to see his knowledge expand beyond “just the science” into the world of cultural competence, relationship-building and Indigenous methodologies of participatory research. I’m excited to continue working with Aidan over the next year and perhaps beyond.