Watch coverage of this story by CTV, Global Television Network and Seattle’s KING5 (NBC).
Three times a week, Calnan Sorenson, age 6, leaves her first-grade classroom in Seattle to work with a teacher for the visually impaired. They spend part of that time introducing her to Braille.
She isn’t blind. The round pink-framed eyeglasses she wears provide minimal visual correction, and she does the things other 6-year-olds do – gymnastics lessons, swimming lessons, impromptu soccer games with her younger brother. But her parents think the Braille lessons are a prudent precaution for the future.
Calnan was born with aniridia, a rare eye disease in which the first and most noticeable symptom is the absence or near-absence of the iris, the coloured part of the eye.
Along with that come several other, more serious and debilitating traits – opaqueness of the cornea, glaucoma (raised pressure inside the eye), and an immature retina, which interferes with colour perception and sharpness of vision.
Like Calnan, most young children with aniridia have reasonably good vision. But their ocular vulnerabilities gradually worsen to the point that as adults, they are usually classified as legally blind – defined by an inability to read the top line on a standard vision chart.
But two University of British Columbia scientists have embarked on an experiment that offers hope for Calnan and other children with aniridia. They are re-purposing a gene-therapy drug that reversed aniridia in mice – a dramatic example, and perhaps the only example ever, of a genetic birth defect being cured through medication.
Now, they are trying the drug on Calnan and 35 others – mostly children – in Canada and the U.S.
“If we start to see some improvement in her acuity or the structure of her eyes in the coming year or years, then, from my perspective, that would be miraculous,” says Calnan’s father, Matt.
Kevin Gregory-Evans, who with his wife, Cheryl, has been working on this treatment for eight years, finds it hard to hold back when discussing the implications of success.

Kevin Gregory-Evans, Professor in the UBC Department of Ophthalmology and Visual Sciences and leader of the clinical trial.
“If we get… benefits in humans anywhere near the effects that we’ve seen in our model systems, I think that this will be unprecedented in medicine and in science,” says Kevin Gregory-Evans, a Professor in the Department of Ophthalmology and Visual Sciences, and the Julia Levy BC Leadership Chair in Macular Research.
He compares the project to treating a child born without a hand.
“What we are thinking we’re going to see in our clinical trial is that by adding a chemical, a simple chemical, we will see re-growth of that hand,” he says. “Not just that the hand becomes useful, but a perfect hand at the end of the treatment regimen – which is unprecedented in medicine, certainly in medicine in the eye.”
Overriding a misplaced “stop sign”
Aniridia, which affects about 5,000 people in North America, is apparent at birth, due to the missing iris. Toddlers with aniridia usually need eyeglasses to see, wear sunglasses or darkened contact lenses to protect their eyes from overexposure to light, and cannot read small text. Their eyes are continually moving, making it difficult for them to focus.
Aniridia is caused by a nonsense mutation – an extra “stop sign” on the gene that interrupts production of a protein, called PAX6, that is crucial for eye development. The truncated protein that results isn’t functional.
Soon after Kevin and Cheryl Gregory-Evans joined UBC in 2009, a New Jersey biotechnology company called PTC Therapeutics developed ataluren, a drug that can override nonsense mutations.
The company is aiming to get ataluren approved for Duchenne muscular dystrophy. Although it has won conditional approval in Europe, disappointing clinical trial results for children with that condition have so far stymied the company’s efforts to get U.S. approval.
Despite that mixed picture, the Gregory-Evans team sought and gained permission from PTC Therapeutics to test the drug on an animal model of aniridia – mice that were genetically engineered to have the PAX6 nonsense mutation. They initially thought the drug would work only in utero – giving it to a pregnant mother to prevent aniridia from arising in her fetus.
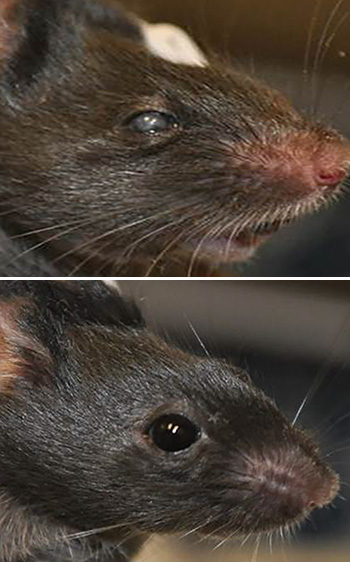
It worked in mice. But the medical and ethical challenges inherent in administering a drug to a human pregnant mother led Cheryl Gregory-Evans, a Professor of Developmental Biology in the Department of Ophthalmology and Visual Sciences, to wonder if it might also work after birth.
“Infectious” enthusiasm
They formulated ataluren into eye drops and applied it to two-week-old mice with aniridia, and found that the drug repaired their damaged eye tissue to 90 per cent of normal, restoring their vision. The results were published in 2013 the Journal of Clinical Investigation.
“We were amazed to see how malleable the eye is after birth,” says Cheryl Gregory-Evans, whose faculty position was funded by an estate gift from the late Sharon Stewart, a Victoria woman with aniridia. “The challenge is getting it to the right place at the right time.”
“We were quite surprised – and I think everybody that has seen the results that we’ve generated has been surprised – by the fact that we see reversal of the disease,” Kevin Gregory-Evans says. “So the hypothesis for our clinical trial work is not that we’re going to suppress progression of aniridia, but that we’re literally – quite literally – going to cure it.”
When Calnan’s father, Matt, heard Kevin Gregory-Evans discuss the animal model results at a conference of Aniridia Foundation International, it was difficult for him to control his excitement.
“His enthusiasm was infectious, and the results he was seeing seemed miraculous,” said Matt, who works as a firefighter in Everett, a Seattle suburb. “As a parent, it’s very easy to get hooked by that, and thinking, ‘We’ve found a cure,’ and I had to resist being tempted by that. But I was very excited just to learn more.”
“You just get over it”
Aidan Gibbons, like so many 11-year-old boys, loves to play soccer – loves it so much, he is willing to play despite his aniridia.
“The ball is really big,” he says. “And I have a good kick, and can run pretty fast. I’m pretty much the same at soccer as other people.”
But from the classroom to the living room, he must make adjustments to his disease.
At school, he needs to sit in the front row to make out the teacher’s writing on the whiteboard, and even then, he depends on devices that will enlarge an image of the board on a tablet at his desk. His teachers give him tests in a larger font. He gets easily tired while reading.
At home, he sits just a meter away from the television, apart from his family on the couch.
“It’s hard for me to see most things that are far away that are other people can see,” he says. “They say, ‘Aidan, look over there!’ But I can’t see it. Sometimes I say, ‘Oh, yeah, I can see it.’ But pretty much I can’t. So that’s a little hard to do, but you just get over it.”
For the most part, he maintains that positive attitude.
“Aidan’s condition never used to bother him, but as he’s getting older, we are noticing comments that he makes about, ‘Oh, if I had better vision, then I could potentially do this,’” says his mother, Kishani. “We continuously remind him that it’s the effort that you put into something, and there are things that he may not be able to do. But there are lots of other things that he can do as well.”
Then one day, Kishani’s sister-in-law saw an article on UBC’s website about the successful experiments on aniridic mice; the article mentioned a forthcoming clinical trial of ataluren.
Kishani, who works in UBC’s building operations department, reached out to Cheryl Gregory-Evans, asking if Aidan fit the criteria for the trial. A few days later, Kishani sent Aidan’s genetic paperwork to Cheryl to determine if he would be a proper fit for the study.
In April 2016, Aidan became what his mother calls “a pioneer in science.”
A medication regimen, and lengthy examinations
Aidan and the other participants in the trial are not getting eye drops, as the mice did, because that would have required proving the safety of that topical form of the drug to U.S. and Canadian regulatory authorities. The powder form, taken orally, already had safety approvals, due to the previous clinical trials for Duchenne muscular dystrophy. So the company and the Gregory-Evans team opted to try an oral powder first.
Three times a day, including once during the school day, Aidan mixes the powder form of ataluren with lemonade and downs the mixture. Four times a year, he comes to Vancouver Coastal Health’s Eye Care Centre for a battery of examinations lasting several hours – reading a vision chart, getting his eyes photographed, getting his eye pressure checked, and, the worst part of all, having a few cells taken from his eye for a biopsy.

Calnan Sorenson, of Seattle, undergoes a vision test during one of her quarterly exams in the clinical trial.
For Calnan, the quarterly visits – which involve a 3- or 4-hour drive north to Vancouver, and an overnight stay at a hotel near the Eye Care Centre – are an opportunity for some daddy-daughter time, including swimming in the hotel pool.
As a reward for submitting to all of the tests, including the painful biopsy, there is the added bonus of a trip to a nearby toy store. As Calnan squirms on an examination chair and Kevin Gregory-Evans gets ready to take a tissue sample, her father reminds her of that bonus.
“This is Toys-R-Us time, my brave girl,” he tells her. “You ready to win the big prize? Put your bottom down.”
Calnan starts giggling. “You said ‘bottom’!”
Matt: “I did, I said ‘bottom.’ Hilarious, right?”
Matt braces her with both of his arms, and Calnan’s legs stiffen as Dr. Gregory-Evans leans in.
Dr. Gregory-Evans: “One, two, three, four, five… Done!”
Matt: “Nice work!”
Calnan lets out a small sob as her dad comforts her. Within a minute, she is back to her playful self.
Moving back from the TV screen
The study is a double-blind randomized controlled trial – neither the participants nor the researchers know who is getting ataluren and who is getting a placebo. It’s also a crossover trial – after a year, everyone will be getting the drug.
Aidan says his eyesight hasn’t improved. But his parents have noticed that he is now sitting farther back from the TV than he used to.
“Or he’s even sitting on the couch, which he would never do,” Kishani Gibbons says. “Although it’s exciting, we don’t focus too much on these incremental changes. I don’t want to give Aidan a sense of false hope. I don’t want to have a sense of false hope… We do explain the importance of his being part of this, not just for him, but for others as well.”
Certainly, there is reason for caution. The results from the clinical trial for children with Duchenne muscular dystrophy did not win over the U.S. Food and Drug Administration (a decision that PTC Therapeutics is appealing). Using the powder form of the drug, taken orally, means the drug is taking a circuitous route to the eye, so there is the possibility that not enough of it is getting to where it needs to go.
“If we are successful, this would be the first time that a genetic disease in the eye was not only stopped, but reversed.”
Kevin Gregory-Evans, UBC Professor of Ophthalmology and Visual Sciences
Kevin Gregory-Evans, however, is optimistic. He notes that achieving positive results with muscular dystrophy is more of a challenge because that is a much more systemic disease than aniridia. He speculates that the aniridic eyes are in a state of “suspended animation,” just waiting for something to jump-start the biological processes that haven’t been taking place for lack of a complete protein. Also, he notes that the animal model of the disease was more severe than the human form, so their dramatic results with mice bode well.
“Verging on science fiction”
Each participant will be in the trial for a little less than two years. Both Calnan and Aidan will be coming up on their one-year anniversaries in April.
Calnan’s father is heartened to see that her eyes haven’t worsened since the trial began.
“If her vision is maintaining and she’s not falling victim to any of those degenerative eye disorders that aniridia can bring on at a young age, then that’s good news,” he says.
But Kevin Gregory-Evans, emboldened by the results he and his wife Cheryl have seen in mice, is aiming higher.
“If we are successful, this would be the first time that a genetic disease in the eye was not only stopped, but reversed,” he says. “Scientifically, it would be astonishing to see such a phenomenon, because we would be doing something that is unprecedented. It’s a concept verging on science fiction, but we’ve seen this in our laboratory, and we’re fairly confident we’ll see the same sort of phenomena, to some extent, in humans.”